Researchers identify key brain circuit regulating cocaine addiction, relapse
When neuroscientists used a molecular brake to stop dopamine signaling in a specific brain circuit, mice previously addicted to cocaine no longer sought the drug
Relapse is a common feature of addiction recovery – two in three patients treated for substance use disorder in the United States relapse within 12 months, according to the Journal of the American Medical Association.
Substances of misuse hijack the brain’s pleasure and reward systems, reinforcing drug-seeking behaviors by flooding the system with “feel good” chemicals, while also producing long-lasting functional changes in brain regions that regulate decisions and motivation.
Combined, these hard-wired biological changes make drug cravings harder to ignore for some, but researchers are developing new ways to prevent relapse by chemically tweaking individual components of neuronal networks, leaving the rest of the brain intact.
In new findings published in Neuron, neuroscientists at the University of California San Diego and the Fralin Biomedical Research Institute at VTC singled out the specific brain circuit that triggers cocaine relapse in mice. When they applied a molecular brake to block activity in this circuit, the mice completely lost their previously avid interest in the drug, resuming normal behavior.
“They went back to baseline – as though they never had been exposed to the drug before,” said Byungkook Lim, associate professor of biological sciences at UC San Diego, and the study’s lead author. “We’ve uncovered a hidden molecular regulator that may play a key role in understanding the tendency to relapse.”
Lim said the finding expands on previous research about how substances of misuse – cocaine, alcohol, tobacco, and other illicit drugs – alter dopamine signaling pathways in the brain, contributing to addiction, a chronic condition that affects 10 percent of American adults, according to the National Institute on Alcohol Abuse and Alcoholism.
The research team, which included co-author Sora Shin, who is now an assistant professor at the Fralin Biomedical Research Institute and in the Department of Human Nutrition, Foods, and Exercise in the College of Agriculture and Life Sciences at Virginia Tech, began the five-year study by examining changes in brain chemical levels after a prolonged period of withdrawal from cocaine.
The scientists focused on the ventral pallidum, a tiny “stepping stone” brain region that connects cortical, amygdalar, and striatal circuits, making it an anatomical hub for encoding rewards, Shin explained. The researchers discovered that cells in this brain area expressed extremely high levels of a certain protein, dopamine receptor D3 (DRD3), two weeks after withdrawal from cocaine.
“This change in brain chemistry wasn’t immediate,” Shin said. “DRD3 production ramped up only after prolonged abstinence, which was a compelling find. This led us to ask: What cells are expressing this protein, and where do they connect in the brain?”
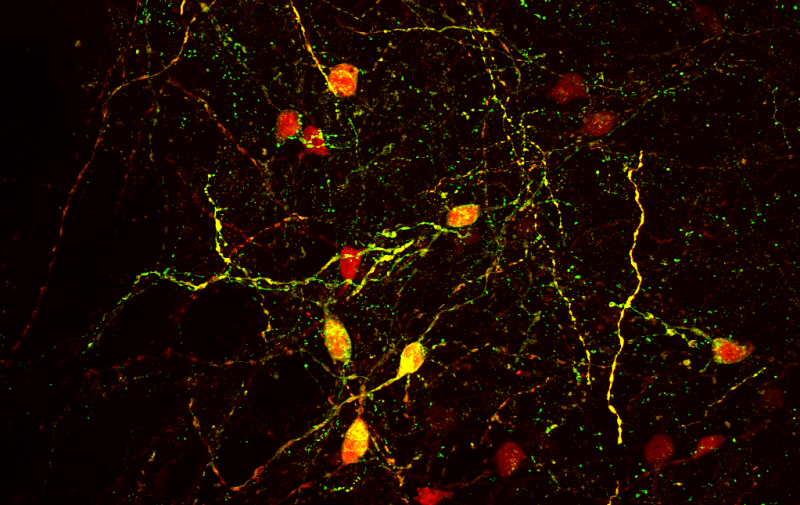
Using a harmless virus to illuminate a neural path, the researchers revealed two locations where these cells connected after leaving the ventral pallidum: the lateral habenula and the ventral tegmental area. Shin developed a genetic knockdown system, targeting a specific molecule, and closely monitored rapid changes in calcium levels in living neuronal cells, allowing her to detect dynamic changes in cellular activity. Combining these techniques, Shin and the other researchers individually compared how these two circuits influenced drug-seeking, and how DRD3 contributes to brain-circuit function.
When the researchers blocked DRD3-expressing neurons connecting the ventral pallidum and lateral habenula, the mice lost complete interest in the cocaine.
Cocaine is a dopamine reuptake inhibitor, which means it floods the brain with dopamine by inhibiting cells from reabsorbing excess dopamine. Previous studies have shown that psychostimulant drugs – such as cocaine and amphetamine – elevate DRD3 expression in several brain regions, in both humans and animals. But this study identifies a specific DRD3 circuit that appears to directly regulate relapse and drug-seeking behavior after a period of abstinence.
“More research is needed, but modulating activity in this specific brain circuit could be effective in preventing drug relapse,” Lim said.
Other authors of the study included Horia Pribiag, Eric Hou-Jen Wang, Fangmiao Sun, Paul Datta, Alexander Okamoto, Hayden Guss, Akanksha Jain, Xiao-Yun Wang, Bruna De Freitas, Patrick Homa, Stefan Pate, and Varoth Lilascharoen, all from UC San Diego; and Yulong Li at the Peking University School of Life Sciences in Beijing, China.




