Expert dispels myths about Lyme disease and offers tips for prevention

Lyme disease is now the most reported vector-borne disease in the United States. It is an infection transmitted by the bite of a tick infected with the bacterium Borrelia burgdorferi.
The Centers for Disease Control and Prevention (CDC) released a report showing that diseases from biting insects, ticks, and mosquitos in the U.S. have tripled since 2004.
Brandon Jutras, a Lyme disease researcher in the College of Agriculture and Life Sciences at Virginia Tech, says, “Warming temperatures are playing an important role in this increase. Ticks not readily killed due to warmer winters, are coming out earlier in the season and spreading to more northern areas. Another factor likely playing a role in the increase is public and physician awareness.”
There are many misconceptions about ticks and Lyme disease, and Jutras, an assistant professor in the Department of Biochemistry and affiliated faculty of the Fralin Life Science Institute, offers several quotes and insights on this issue.
MYTH: All ticks transmit Lyme disease.
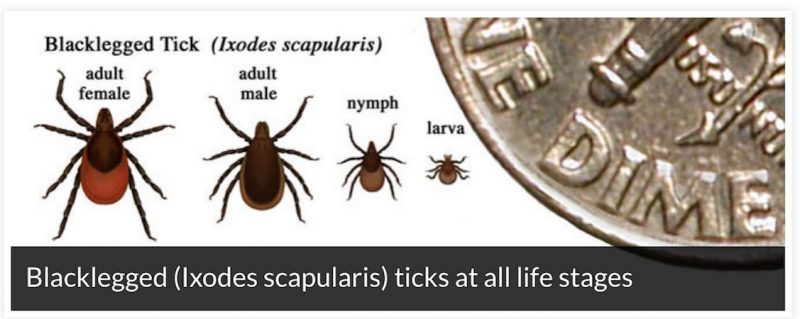
“Four major species of ticks are capable of transmitting the bacteria that causes Lyme disease, only one of which is found in our area: the blacklegged, or deer tick, Ixodes scapularis. It spreads the disease in the northeastern, mid-Atlantic, and north-central United States. The western blacklegged tick, Ixodes pacificus, is responsible for transmitting the disease on the Pacific Coast, and in Europe and Asia, Ixodes Ricinus and Ixodes persulcatus ticks act as vectors of Lyme disease. That said, Virginia is home to a few other species of ticks that transmit other diseases.”
“It is also important to remember that just because you are bitten by a tick, doesn’t mean the tick is carrying the bacteria that causes Lyme disease. Also, the duration of tick attachment, or feeding time, is important. B. burgdorferi lives in the gut of the tick, but is transmitted through the saliva. Once the tick bites, the bacteria have a rather long journey, which can take anywhere from 12 to 72 hours to be transmitted, so prompt removal is critical.”
MYTH: Burning or salting ticks is the only way to remove them.
“NO! This can actually make matters worse. The only appropriate way to remove a tick is to get as close to your skin as possible with fine tweezers and pull. Any other method, including grabbing the tick by the body can actually accelerate the transmission process, increasing the chances of infection. Commercially available tick removers are also available and are effective.”
MYTH: All ticks actively search for hosts.
“Many ticks do not display typical host-seeking behavior — that is to say, they don’t chase you like mosquitoes. Virtually all blood-feeding arthropods sense their hosts by the carbon dioxide they emit when breathing. As a result, they can locate and actively seek out their host. Unlike some tick species that are aggressive host seekers like the Lone Star tick, the Ixodes ticks that transmit Lyme disease are different in that they are more passive--they sit and wait for you to brush by. That’s why it’s important to check yourself often when doing any outdoor activities like gardening, hiking, or any activity that involves longer grass near wooded areas and leaf litter.”
MYTH: I would know if I were bitten by a tick.
“This is common assumption, but not necessarily true. During feeding, ticks are slowly injecting a very complex mixture of salivary components, a few of which act to numb the area. So, unlike a mosquito, most people don’t feel a tick feeding, unless you happen to be allergic to one of the salivary components. The other issue is their size. The second stage, nymph, is about the size of a pencil tip. You often have to feel for them because some life stages are not obvious. Finally, Ixodes ticks tend to be a little picky as to where they actually feed. They seem to enjoy warm, moist areas like the groin, back of the knee, or armpit, which are not obvious or easy places to check regularly.”
MYTH: Everyone with Lyme disease gets a telltale bull’s eye rash
“While the history of Ixodes tick bite followed by presentation of a bull’s eye rash, Erythema migrans, is a clear indication of Lyme, not everyone who contracts the disease will develop this rash. The rash is thought to be an immune response to the bacteria as they begin moving throughout the body. But, immune responses can vary. As a result, it is estimated that 20 to 30 percent of people who acquire Lyme disease DO NOT get the typical rash.”
MYTH: If the test is negative, you don’t have Lyme disease.
“If you have symptoms, you should go to a physician right away. The best diagnostic for Lyme disease is a blood test which measures a patient’s serum for specific antibodies produced in response to certain bacterial products. This type of response can take 1-2 weeks to detect since the body must develop sufficient amounts of antibody, or, titer, to allow for faithful detection. So, if you were bitten in an area where the tick is prevalent and you continue to have symptoms of Lyme disease, it is often worth a second trip to see your physician if you did not have detectable titers immediately.”
Tips for Prevention
“Wear light-colored clothing while enjoying the outdoors and treat these clothes with DEET, or N,N-diethyl-meta-toluamide, containing bug spray. This does work well at repelling ticks, and light colored clothing will allow you to spot the ticks more easily. When in high risk areas check yourself often, initial tick contact almost always occurs below your thigh.”
“If you’ve been bitten, don’t panic, promptly and carefully remove the tick and save it. The tick can be useful in possible future diagnostic efforts.”
“On hikes, or in my car glove box, I carry a fine-tipped pair of tweezers and a small container, the size of a pill bottle, with over the counter rubbing alcohol, or, 70 percent ethanol. Use the tweezers to remove the tick, and drop it into the container with alcohol to kill and preserve the tick should testing be required in the future.”
“Our furry friends are wonderful companions, but they are tick magnets! Commercial tick treatments often prevent attachment, and will usually kill the ticks if they do start feeding, but they do not prevent contact. What happens? Often the ticks are brought inside from the outdoors by our pets and they are then able to bite us. So, check your pets often. It is not only good practice because the commercial treatments work well, but are not 100 percent effective, and it can help you and your family stay safe.”
“Don’t skip the dryer. Spring and summer weather encourages many people to hang their clothes to dry. However, ticks survive the washer and can remain on clean clothes. They do not, however, survive the dryer! If you have returned from a high risk activity, like hiking or camping, be sure to use the dryer on all articles of clothing.”
Brandon Jutras is an assistant professor of biochemistry in the Virginia Tech College of Agriculture and Life Sciences. His research examines ticks and Borrelia burgdorferi, the spirochetal bacterium that causes Lyme disease. During his 10+ years of studying Lyme disease, he has published more than 15 peer-reviewed articles in many of the research community’s top journals. His lab is currently using molecular and cellular techniques to develop new diagnostic tools and therapies for the treatment of Lyme disease in addition to researching Lyme arthritis in the late stages of the disease.
- Written by Kristin Rose
Expertise featured in ABC News and WVTF (NPR affiliate).
Schedule an interview
To interview Brandon Jutras, contact Ceci Leonard by email at ceciliae@vt.edu or by phone at 540-357-2500.
Our studio
Virginia Tech's television and radio studios can broadcast live HD audio and video to networks, news agencies, and affiliates interviewing Virginia Tech faculty, students, and staff. The university does not charge for use of its studios. Video is transmitted by LTN Global Communications and fees may apply.